
Preserving a patient's legacy - Harold's story…
Harold was a patient with metastatic bowel cancer - he had just months to live. Over his lifetime, he had been instrumental in transforming acres of farmland into the village that he grew to love. This legacy was extremely important to Harold. In an effort to keep this heritage alive, he had large posters made of photos, and he even used his carpentry skills to create an entire model of the town. Upon hospice visits, his only focus was teaching his caregivers about this legacy; he did not want it lost with his death.
His caregivers began videotaping him sharing the story of his village – but that wasn't enough for Harold. With his permission, a local TV station was brought in, focusing on the model, photos, and the stories behind them. The TV personnel never mentioned that Harold was ill. The video aired on the local station, and Harold was ecstatic - and at peace. He passed away soon after, his legacy preserved.
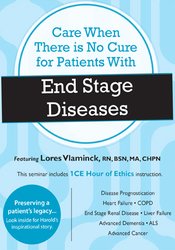
In this compelling recording, multiple case studies like Harold's will provide you with examples that you can incorporate when caring for the terminally ill. Caring for patients with end stage disease requires extreme sensitivity, deep compassion, and extraordinary knowledge. In order to deliver expert, holistic care, healthcare professionals need to have a toolbox full of new interventions to promote quality of life.
Each particular end stage disease has unique complexities for the patient, the family, and the healthcare professional - and this recording will cover specific strategies for caring for these patients.
Did you know that a patient seeking a liver transplant can be on hospice care while waiting? We will discuss how this is done.
What can we do for patients with COPD who's seemingly only solution for an exacerbation is a visit to the ER? We have an intervention for this.
How can we keep costs down without sacrificing patient care? We’ll give you the latest strategies, proven successful in practice.
It's time to think outside the box.
Walk away from this recording with new tools for quality support - and care when there is no cure.

Lores J. Vlaminck, MA, BSN, RN, CHPN, LALD
Principal, Lores Consulting, LLC
Lores Consulting, LLC has been a leading provider of consulting, training, and mentoring for hospice, assisted living, home care and related health care providers for the past 17 years. "Lores has the heart of a teacher, and her passion is to support others in the hospice, palliative, and the home care industry."
Lores Consulting, LLC provides providers with education training and mentoring as well as mock surveys, agency analysis and audits. Drawing on her 45 years of nursing experience, Lores seeks to empower all her client providers to utilize their skills and expertise to reach their greatest potential. Her extensive nursing background includes clinical practice in cardiac and intensive care, outpatient clinic services, as well as serving as a home care and hospice administrator/director for 19 years in greater Minnesota.
In addition to being a certified hospice and palliative care nurse, Lores is also a trainer for the End-of-Life Nursing Education Consortium (ELNEC) curriculum that encompasses palliative and hospice care. She was named the "2010 Geriatric ELNEC Educator of the Year" by ELNEC.
Speaking topics include end-of-life care, grief and loss, compassion fatigue, professional boundaries, pain and symptom management, and many health and employee related topics. Lores also offers national, international consulting and mentoring services – encompassing education, training and compliance evaluations – to hospice and home care agencies, assisted living providers, and long-term care facilities.
As Principal of Lores Consulting, LLC, Lores sees her company’s mission to coach and encourage care providers to work to the ‘top of their license’ to ensure excellence in their delivery of care.
Currently, Lores serves as a board member of three non-profit health care organizations, and is a national speaker for PESI Healthcare and ELNEC. Lores is a graduate of Bethel University in St Paul, MN and holds a Bachelor of Science degree in nursing, as well as a master’s degree in nursing education.
Speaker Disclosures:
Disease Prognostication: An Inexact Art & Science
Congestive Heart Failure: The Broken Heart
Chronic Obstructive Lung Disease
Renal Disease
Liver Disease
Advanced Dementia
Amyotrophic Lateral Sclerosis
Advanced Cancer
Eight Signs of Impending Death
Challenging Decisions
Moral Distress
Please wait ...